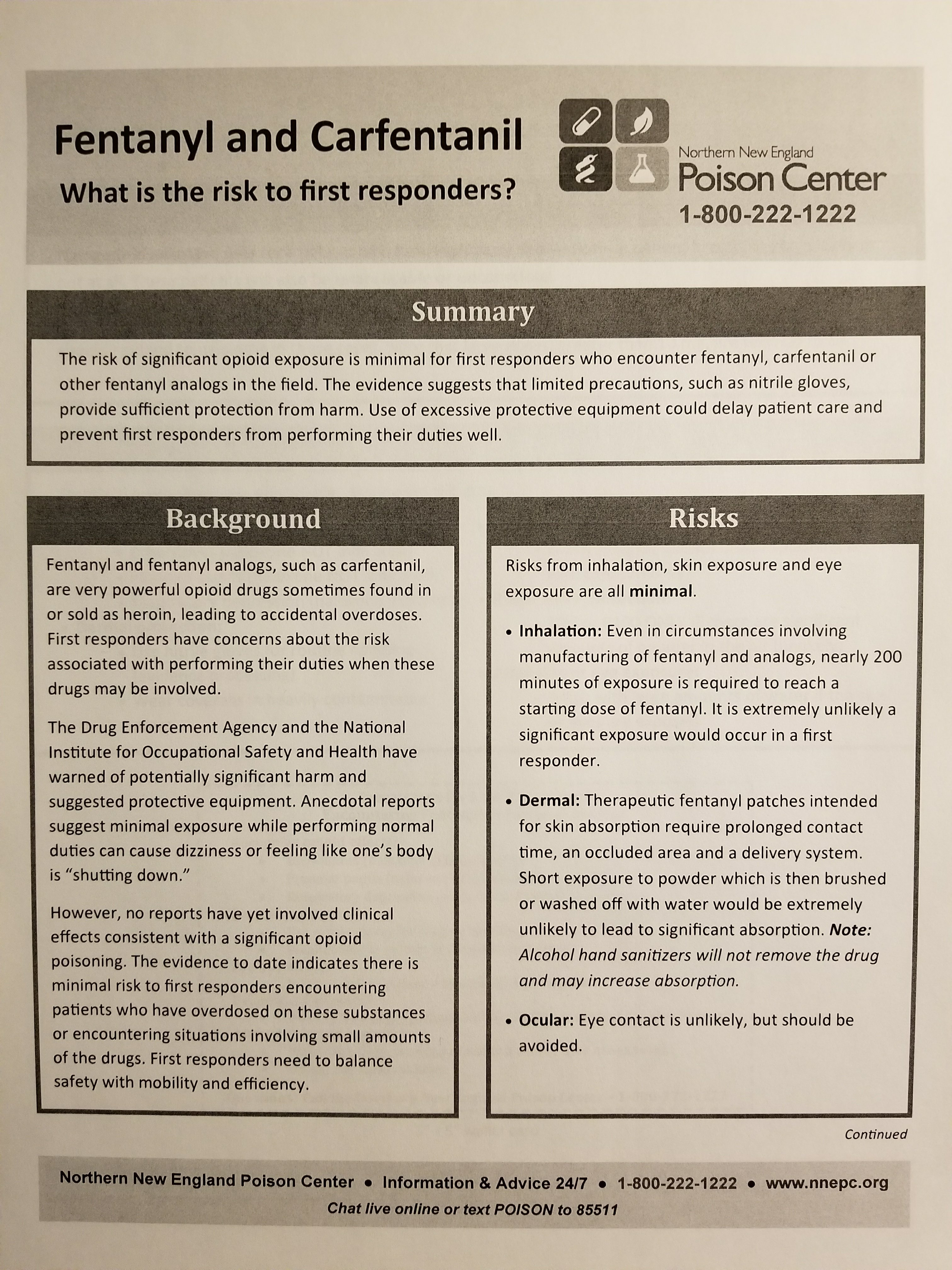
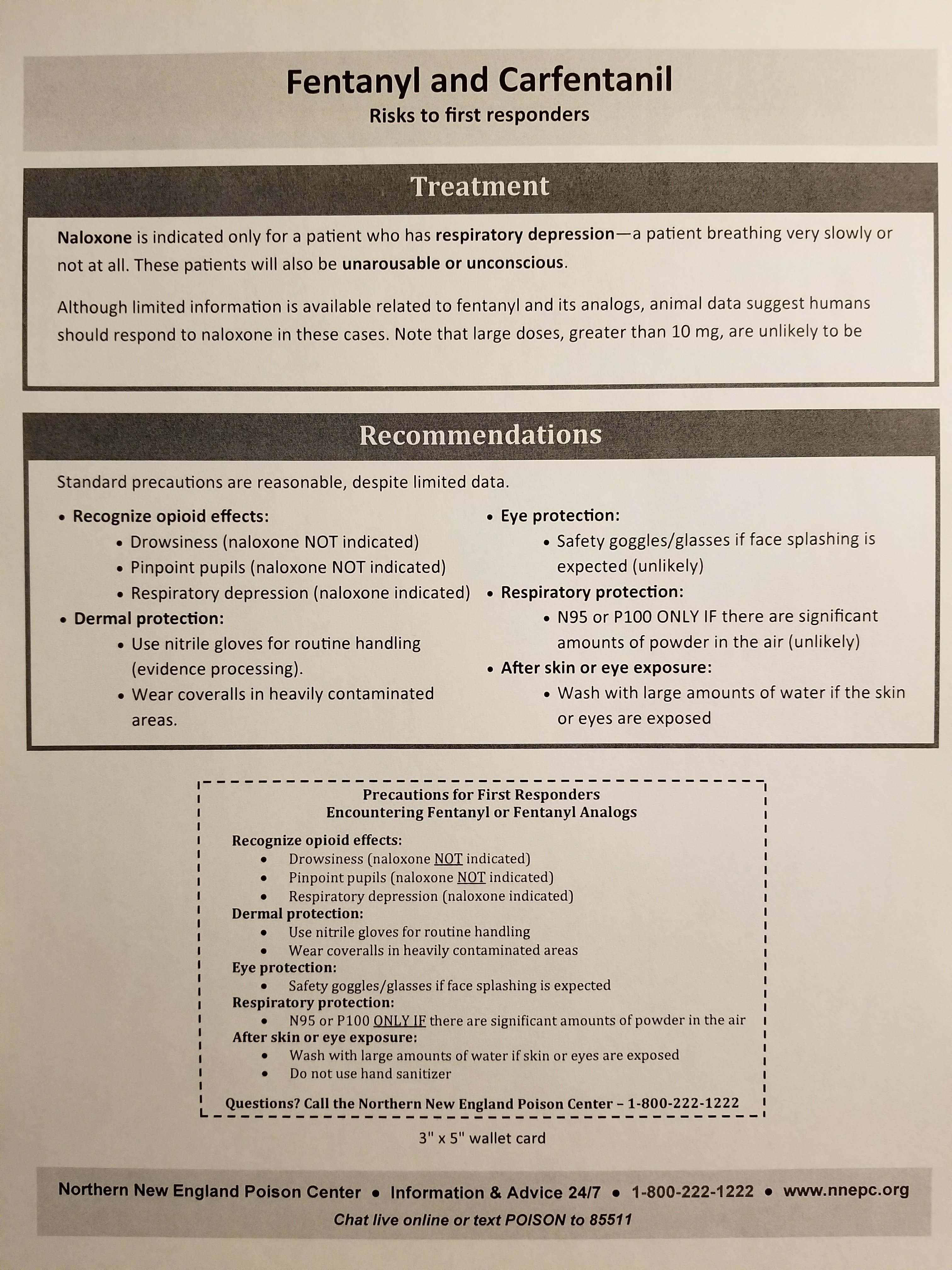
From the Northern New England Poison Control: “The risk of significant opioid exposure is minimal for first responders who encounter fentanyl, carfentanil or other fentanyl analogs in the field. The evidence suggests that limited precautions, such as nitrile gloves, provide sufficient protection from harm. Use of excessive protective equipment could delay patient care and prevent first responders from performing their duties well.”
Sensationalistic articles are popping up like wildfire about Fentanyl exposure. So how on earth have Paramedics and Nurses been able to give Fentanyl and Duragesic Patches to patients for decades without dying of overdoses? It’s astounding any of us have survived!
Look, the hype and hysteria is just that. Touching a drawer handle isn’t going to make you weak-kneed and give you headaches and make you feel like you will pass out. You’re awake and fully lucid one second and lying on the floor the next. That’s just not reality. What we seem to be missing from all these reports are toxicology labs proving Fentanyl is the culprit. I have no doubt some of these cases are psychosomatic due to the stigma over Fentanyl and its cousins, like Carfentanil.
Are the drugs dangerous? Sure, with extensive exposure and even injection of high doses.
Should we be concerned with exposure? Yes, but no more so than with contracting Hep C, influenza, or any other communicable pathogen.
Now, the Northern New England Poison Control has released some solid, common sense guidance on dealing with Fentanyl (and related drugs) exposure, and NOTE the guidance on administration of Narcan (naloxone). Only for RESPIRATORY DEPRESSION! Not for any other symptom! This is what proper use of Narcan is for. Not for pinpoint pupils, not for fatigue, not for weakness, and NOT AS A PREVENTATIVE MEDICATION “just in case” you come across Fentanyl.
Download the .pdf flyer on Fentanyl and please pass it arpund as a memo to your department, and train on this too!
http://www.nnepc.org/shop/fentanyl-carfentanil-fact-sheet-for-first-responders
Here are some photos of the document:
EDIT: The following information is the position of the nation’s boards of toxicology experts:
ACMT and AACT Position Statement: Preventing Occupational Fentanyl and Fentanyl Analog Exposure to
Emergency Responders
The position of the American College of Medical Toxicology (ACMT) and American Academy of Clinical Toxicology
(AACT), is as follows:
Fentanyl and its analogs are potent opioid receptor agonists, but the risk of clinically significant exposure to
emergency responders is extremely low. To date, we have not seen reports of emergency responders developing
signs or symptoms consistent with opioid toxicity from incidental contact with opioids. Incidental dermal absorption is unlikely to cause opioid toxicity. For routine handling of drug, nitrile gloves provide sufficient dermal protection. In exceptional circumstances where there are drug particles or droplets suspended in the air, an N95 respirator provides
sufficient protection. Workers who may encounter fentanyl or fentanyl analogs should be trained to recognize the
signs and symptoms of opioid intoxication, have naloxone readily available, and be trained to administer naloxone and provide active medical assistance. In the unlikely event of poisoning, naloxone should be administered to those with objective signs of hypoventilation or a depressed level of consciousness, and not for vague concerns such as dizziness or anxiety. In the absence of prolonged hypoxia, no persistent effects are expected following fentanyl or fentanyl analog exposures. Those with small subclinical exposures and those who awaken normally following naloxone administration will not experience long-term effects. While individual practitioners may differ, these are the
positions of American College of Medical Toxicology and American Academy of Clinical Toxicology at the time written, after a review of the issue and scientific literature.
https://www.acmt.net/_Library/Fentanyl_Position/Fentanyl_PPE_Emergency_Responders_.pdf


